Issues with cortisol occur in some CFS patients but is not a frequent condition. To me this implies that it is either DNA related or microbiome related.
- Mild hypocortisolism (low cortisol) with attenuated diurnal variation has also been reported in some patients with CFS [2011].
- especially prone in women to support chronically depressed cortisol levels and a persistent inflammatory signature consistent in some CFS populations [2014].
- We concluded that depressed salivary cortisol may be an uncommon factor in CFS as even in those cases where it might play a role it did not persist despite persistence of symptoms [2013].
So which is it — or is it both? The literature indicates that it is influence by stress and has impact on the microbiome.
- Hypocortisolism and increased glucocorticoid sensitivity of pro-Inflammatory cytokine production in Bosnian war refugees with posttraumatic stress disorder[2004].
- Infectious causes of adrenal insufficiency [2003].
- A study with dogs suggest that there is a DNA component “The data supports the existence of breed-specific differences in incidence rates of naturally occurring adrenocortical insufficiency (NOAI) in dogs.”[2016]
“Endocrine pathways such as the hypothalamic-pituitary-adrenal (HPA) axis act as links between the nervous and the immune system via cortisol. In turn, the nervous system is linked to the gut by the vagus nerve as a feedback system for the autonomous gut innervation. In addition, cytokine patterns might play a crucial role in the psychoneuroimmunlogical interplay between gut and brain. These patterns might be altered by cortisol shifts as observed under chronic stress conditions. The immunosuppressive effect of cortisol might also affect the conditions at the gut epithelium as well as gut bacterial composition [2013].”
- Prebiotic intake reduces the waking cortisol response and alters emotional bias in healthy volunteers[2015]. “The salivary cortisol awakening response was significantly lower after Bimuno®-galactooligosaccharides intake compared with placebo.”
Reviewing the literature finds that adaptogens appears to be the herbs of choice for dealing with high cortisol issues. Thus by inference, they should be avoided with low cortisol. This inference may be wrong — their may be normalizer which work on both side of cortisol shifts. For one, Licorice, it doubles the half-life of cortisol (i.e. keep it around longer which implies that it may raise the level).
Wikipedia lists the following:
“There is dispute in the herbal community regarding whether certain plants qualify as adaptogens. However, certain plants are generally believed to qualify:
- American Ginseng (Panax quinquefolius), root[11]
- Ashwagandha (Withania somnifera), root[12]
- Asian Ginseng (Panax ginseng), root[13]
- Cordyceps (Cordyceps sinensis), mushroom/mycelium
- Dang Shen (Codonopsis pilosula, C. tangshen), root
- Eleuthero (Eleutherococcus senticosus), root/stem bark
- Guduchi (Tinospora cordifolia), root/stem
- Holy Basil (Ocimum sanctum, O. gratissimum), herb — aka TULSI
- Jiaogulan (Gynostemma pentaphyllum), herb
- Licorice (Glycyrrhiza glabra, G. uralensis), root
- Reishi (Ganoderma ludicum), mushroom/mycelium
- Rhaponticum (Rhaponticum carthamoides), root
- Rhodiola (Rhodiola rosea), root
- Schisandra (Schisandra chinensis), fruit/seed
- Shilajit (Asphaltum bitumen), pitch [14]“
I have high lighted in red the items that I have cited on this blog.
Bottom Line
Traditionally low cortisol was associated with mycobacterium tuberculosis infections, thus the microbiome seen with such patients may hint at the bacteria associated with low cortisol.
- “Phylum-level analysis showed that the relative abundance of Firmicutes and Actinobacteria was significantly higher in TB samples and Neisseria and Veillonella were two dominant genera after Streptococcus.”[2016]
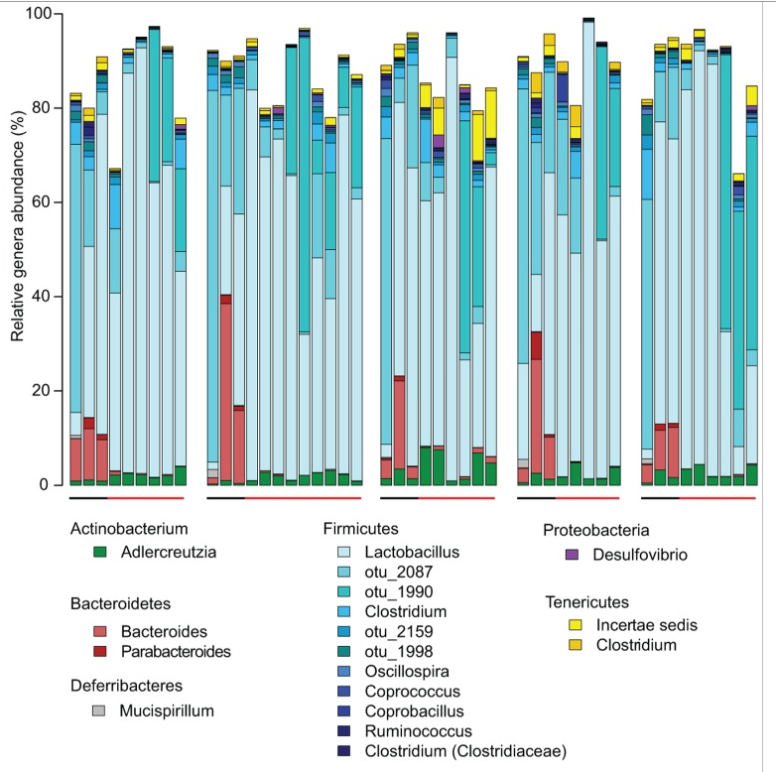
- Aerosol Mycobacterium tuberculosis infection causes rapid loss of diversity in gut microbiota [2014]. [Full Text] Below is a chart showing how bacteria shifted during the course of TB
- Treatment addressing the root cause is largely unknown except that the root cause appears to be largely due to a bacteria shift, a specific subset of bacteria that is not common across CFS patients.
What is really needed is a good study of the microbiome of patients with low cortisol levels. Until then, my best suggestion is: GeneralBiotics Equilibrium, Prescript Assist and Bifidobacteria probiotics.
